Introduction
Radiotherapy plays an important role in cancer treatment, as it aims to deliver precise doses of radiation to target tumours while sparing surrounding healthy tissue. Over the years, advances in computational dosimetry have revolutionized the field, allowing for more personalized and effective treatment plans. In this publication, we will explore some of the key advances in computational dosimetry and their impact on improving patient outcomes.
3D Treatment Planning

Traditional radiation therapy planning was predominantly based on 2D imaging, limiting the accuracy of dose delivery. However, with the advent of computed tomography (CT) and magnetic resonance imaging (MRI), clinicians can now create detailed 3D models of the patient’s anatomy. These high-resolution images enable precise delineation of tumour volumes and nearby critical structures, optimizing treatment plans.
Monte Carlo Simulations
Monte Carlo simulations have become a cornerstone of computational dosimetry, providing a comprehensive and precise method to calculate radiation dose distributions. Unlike traditional algorithms, Monte Carlo simulations simulate individual radiation interactions, offering a more realistic representation of dose deposition in tissues. This advancement ensures more accurate predictions and helps refine treatment plans for better outcomes.
Biological Models and Radiobiology

Integrating biological models and radiobiological data into computational dosimetry has advanced our understanding of how different tissues respond to radiation. By taking into account the variable sensitivities of tumors and healthy tissues, treatment plans can be optimized to achieve maximum tumor control while minimizing side effects on healthy tissues. This approach, known as biological dose optimization, has significantly improved treatment outcomes.
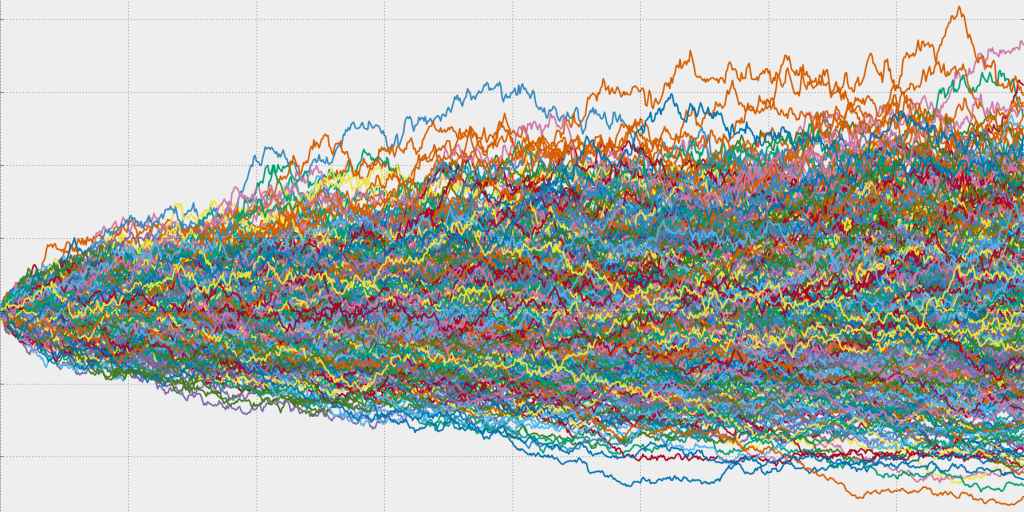
Adaptive Radiation Therapy
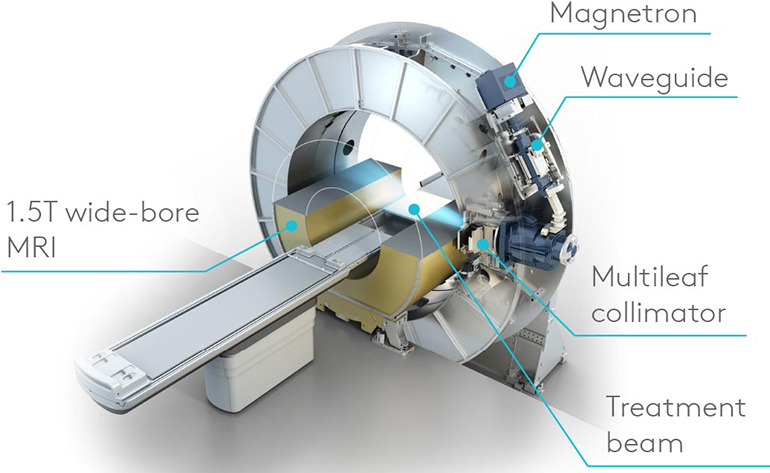
One of the most important developments in computational dosimetry is the concept of adaptive radiotherapy (ART). With ART, treatment plans are dynamically modified based on changes in tumour size, shape, and position over the course of treatment. This real-time adaptation ensures that the radiation dose remains optimal, even as the tumour evolves, ultimately increasing treatment efficacy.
Conclusion
Advancements in computational dosimetry have brought about a paradigm shift in radiation therapy. The integration of 3D treatment planning, Monte Carlo simulations, radiobiological data, and adaptive techniques has led to more precise, personalized, and effective treatment strategies. These innovations continue to shape the future of cancer care, providing patients with improved outcomes and a higher quality of life.
Author: Abdelhai Ben Ali, PhD
Supporting Documents
- McNutt T. Advances in computational radiation dosimetry. Seminars in Radiation Oncology (2018). DOI: 10.1016/j.semradonc.2017.10.002
- Sgouros G., Hobbs R. Advances in computational dosimetry for radionuclide therapies. Medical Physics (2018) DOI: 10.1002/mp.12989
- Xu X. G. Monte Carlo and deterministic radiation transport simulations: A comparison of efficiency and accuracy for radiation dosimetry applications. Health Physics (2013). DOI: 10.1097/HP.0b013e31827a6810
