Introduction
Radiation treatment is a crucial method for fighting cancer, and to make it more effective and safe, medical physicists use computational models. These models are like powerful calculators that help them design the best treatment plan for each patient. In this article, we’ll explore how these models work and why they are essential for radiation treatment planning..
What are Computational Models?
Computational models are virtual representations of the human body and its tumour. Medical physicists use advanced mathematics and computer algorithms to simulate how radiation beams interact with cancer cells. Think of it as a “pretend” version of the patient’s body inside a computer, where doctors can test different treatment scenarios.
Evaluating Treatment Options
Before starting treatment, medical physicists can use computational models to evaluate different radiation techniques and treatment options. They can compare various scenarios and select the one that has the best chance of success for each patient’s unique situation.
Personalizing Treatment Plans
Every patient is unique, and their cancer is different from others. Computational models take into account the patient’s specific anatomy, tumour size, and location. By personalizing the treatment plan, doctors can target cancer more accurately while minimizing damage to healthy tissues around it.
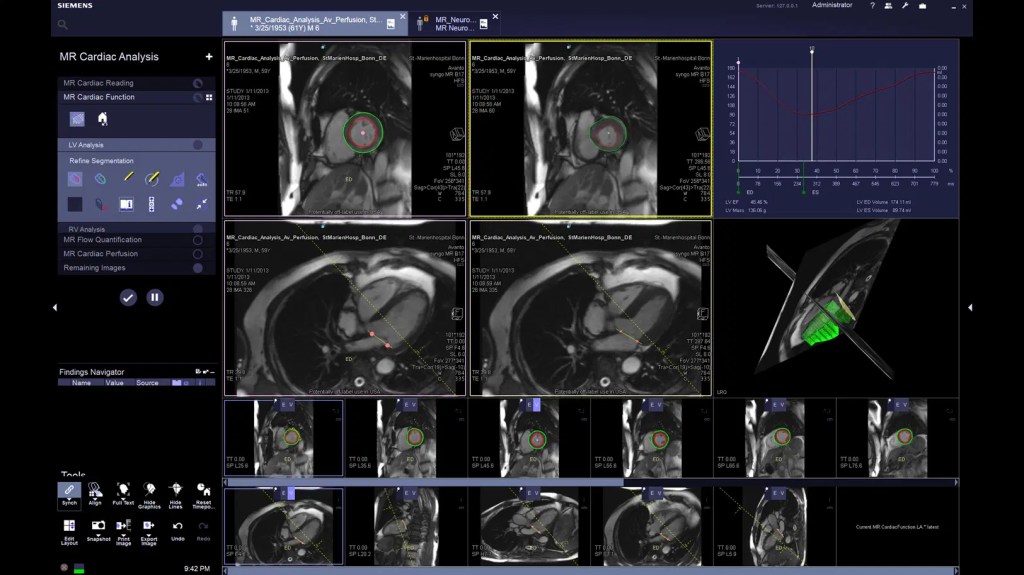
Enhancing Treatment Precision
Precision is extremely important in adiation treatment. Computational models enable medical physicists and doctors to visualize the radiation beams’ paths and how they will interact with the tumour. This precision ensures that the radiation reaches the cancer cells while sparing healthy tissues as much as possible.
Optimizing Radiation Dose
Determining the right amount of radiation to deliver to the tumor is crucial. Too little radiation might not effectively kill the cancer cells, while too much could harm healthy organs nearby. Computational models help doctors find the optimal radiation dose, striking the right balance between effectiveness and safety.
Reducing Side Effects
By using computational models, medical physicists and doctors can predict the potential side effects of radiation treatment more accurately. This information helps them adjust the treatment plan to reduce side effects and improve the patient’s quality of life during and after treatment..

Conclusion
Computational models play a vital role in radiation treatment planning by providing medical physicists and doctors with powerful tools to design personalized and precise treatment plans. Through these models, radiation therapy becomes more effective in fighting cancer while minimizing harm to healthy tissues. Embracing these advanced technologies brings hope for better outcomes and improved patient care in the battle against cancer.
Author: Abdelhai Ben Ali, PhD
Supporting documents
- M. Le, Herve D. J. Kalpathy-Cramer, E. R. Gerstner et al. Personalized Radiotherapy Planning Based on a Computational Tumor Growth Model. IEEE Trans Med Imaging. 2017 Mar;36(3):815-825. doi: 10.1109/TMI.2016.2626443. Epub 2016 Nov 8.
