Introduction
Proton therapy, a cutting-edge technology in cancer treatment, offers better accuracy and fewer side effects than older radiation methods, giving new hope to cancer patients. In this article, we’ll dive into the basics of proton therapy, its benefits, and how it’s changing cancer treatment. We’ll also explore recent scientific advancements like calculating treatment range, adjusting therapy as needed, controlling for patient movement, and using genomics and computer science to make proton therapy even better.
What’s the Basic of Proton Therapy?
Proton therapy utilizes protons, positively charged particles, to precisely target cancer cells. Unlike conventional X-ray radiation, protons can be controlled to release their energy at a specific depth within the body, minimizing damage to surrounding healthy tissues. This targeted approach significantly reduces the risk of long-term side effects, making proton therapy an attractive option for treating various cancers.
How Versatile is Proton Therapy in Cancer?
Proton therapy has shown promise in treating a variety of cancers, including brain tumors, prostate cancer, lung cancer, and pediatric cancers. Its ability to spare surrounding healthy tissues is particularly beneficial in cases where tumors are located near critical structures or in pediatric patients, where minimizing long-term side effects is of utmost importance.
What Advances Aid Proton Therapy Accessibility?
Initially, proton therapy was limited to a few specialized centers. However, as technology has advanced, more facilities are incorporating proton therapy into their cancer treatment programs. This increased accessibility is expanding the reach of this innovative therapy, offering new hope to a broader range of patients.
Dosimetry Challenges and Solutions
Accurate dosimetry is critical in proton therapy to ensure the prescribed dose is delivered precisely to the target volume. Researchers are addressing dosimetric challenges, such as range uncertainties and biological variations. Advances in imaging modalities, such as cone-beam CT and MRI, aid in real-time imaging during treatment, contributing to improved dose delivery accuracy.
Technological Advances in Proton Therapy
Proton therapy relies on sophisticated technology for precise treatment delivery. The latest proton therapy facilities boast advancements in proton beam delivery systems, including pencil beam scanning (PBS) and intensity-modulated proton therapy (IMPT). These technologies allow for highly conformal dose distributions, enabling targeted treatment while sparing adjacent healthy tissues.
Radiobiological Considerations
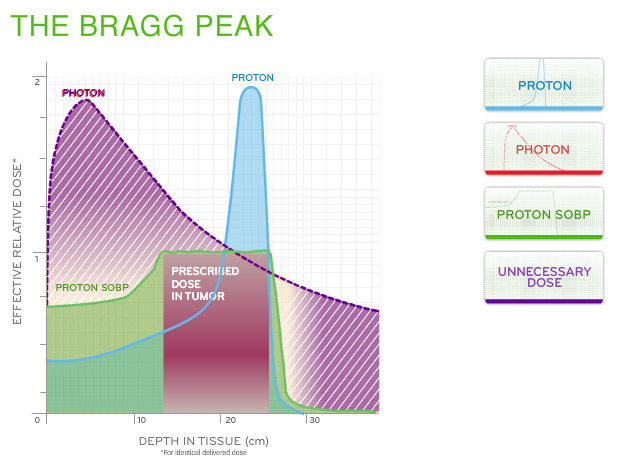
Understanding the radiobiological effects of proton therapy is a key focus for medical physicist researchers. Protons deposit their energy in a defined region, known as the Bragg peak, offering an advantage in sparing healthy tissues compared to traditional radiation. Ongoing research investigates the radiobiological implications of this unique energy deposition profile, exploring its impact on tumor control and normal tissue toxicity.
Clinical Trials and Outcomes Research
To validate the efficacy of proton therapy, ongoing clinical trials are essential. Medical physicist researchers contribute to the design and execution of these trials, evaluating proton therapy in various cancer types and comparing outcomes with conventional radiation modalities. This research is crucial for establishing evidence-based guidelines for the clinical implementation of proton therapy.
Integrating Genomics and Bioinformatics
The advent of genomics and bioinformatics has opened new avenues for personalized cancer treatment. Understanding the genetic makeup of tumors allows for the identification of specific molecular targets. Proton therapy, when integrated with genomics, enables the delivery of highly targeted treatment tailored to the individual characteristics of the tumor. This approach holds promise for increased treatment efficacy and reduced side effects.
AI/ML in Proton Therapy
Artificial intelligence and machine learning play a pivotal role in optimizing proton therapy. These technologies aid in treatment planning, predicting treatment outcomes, and adapting treatment in real-time. AI algorithms analyze vast datasets, identifying patterns and optimizing treatment plans for individual patients. The synergy between AI/ML and proton therapy is at the forefront of advancing precision medicine in cancer treatment.
Challenges and Future Directions
While proton therapy holds great promise, challenges persist, including the high cost of facility construction and the need for increased accessibility. Medical physicists are actively involved in addressing these challenges and exploring novel technologies, such as compact proton therapy systems and FLASH proton therapy, which delivers doses in ultra-high dose rates.
Why Choose Proton Therapy for Precision?
One of the primary advantages of proton therapy is its precision. Traditional radiation therapy, while effective, may inadvertently affect nearby healthy tissues and organs. Proton therapy’s ability to precisely control the depth of radiation allows for a more targeted approach, reducing the risk of side effects and improving the overall quality of life for patients during and after treatment.
Does Proton Therapy Improve Clinical Efficacy and Reduce Side Effects?
Clinical studies have demonstrated the efficacy of proton therapy in achieving similar or even improved cancer control rates compared to traditional radiation therapies. Moreover, the reduced exposure of healthy tissues to radiation has resulted in fewer side effects, making proton therapy a favorable option for certain patient populations.
Advanced Range Calculation
Accurate range calculation is crucial for the success of proton therapy. Recent advancements in imaging technologies, such as positron emission tomography (PET) and magnetic resonance imaging (MRI), have enabled more precise determination of tumor boundaries. Additionally, Monte Carlo simulations and advanced treatment planning systems contribute to improved range calculation, ensuring that the protons reach the desired depth within the tumor.
What’s Adaptive Proton Therapy’s Impact?
The dynamic nature of tumors requires adaptive treatment strategies. Adaptive proton therapy involves modifying the treatment plan based on changes in the tumor’s size, shape, or location during the course of treatment. This real-time adjustment ensures that the treatment remains optimally effective, particularly in cases where tumors may shrink or move over time. Adaptive techniques enhance the ability to respond to the evolving nature of cancer, improving treatment outcomes.
Treatment Planning Strategies
Medical physicist researchers are actively engaged in refining treatment planning algorithms for proton therapy. Robust optimization techniques are evolving to account for uncertainties in patient setup and anatomical changes over the course of treatment. Moreover, research is ongoing to explore the integration of artificial intelligence and machine learning in treatment planning, optimizing dose distributions based on patient-specific characteristics and historical data.
Dosimetry Challenges and Solutions
Accurate dosimetry is critical in proton therapy to ensure the prescribed dose is delivered precisely to the target volume. Researchers are addressing dosimetric challenges, such as range uncertainties and biological variations. Advances in imaging modalities, such as cone-beam CT and MRI, aid in real-time imaging during treatment, contributing to improved dose delivery accuracy.
Treatment Adaptation and Personalization
Adaptive proton therapy is an emerging area of interest for medical physicists. Researchers are exploring strategies for adapting treatment plans based on real-time imaging, allowing for modifications to account for changes in tumor size, shape, or position during the course of treatment. Personalized proton therapy, considering individual patient characteristics and genomics, is a frontier that holds promise for optimizing treatment outcomes.
Challenges and Ongoing Research
While proton therapy represents a significant leap forward, challenges remain. These include the high initial costs of building proton therapy facilities and ongoing research to refine treatment protocols. Researchers are also investigating ways to integrate proton therapy with other treatment modalities to further enhance its effectiveness.
Combining Proton Therapy with Immunotherapy
The intersection of proton therapy and immunotherapy is a burgeoning field. Researchers are investigating how proton therapy may influence the tumor microenvironment, potentially enhancing the efficacy of immunotherapeutic interventions. The interplay between radiation and the immune system opens new avenues for combination therapies, with implications for improved cancer control.
Conclusion
Proton therapy, as a field of research, is poised for further growth, with much research focusing on leveraging advanced techniques such as precise range calculation, genomics, and the integration of AI/ML. The potential lies in enhancing treatment outcomes and reducing side effects. This future direction embodies the promise of more effective, personalized cancer therapies and symbolizes the advancement of modern oncology research.
Author: Abdelhai Ben Ali, PhD
Supporting documents
- ICRU 1998 Clinical proton dosimetry: I. beam production, beam delivery, and measurement of absorbed dose ICRU Report 59 (Oxford: Oxford University Press).
- Paganetti H. Nuclear interactions in proton therapy: dose and relative biological effect distributions originating from primary and secondary particles Phys. Med. Biol. (2002) 47 747–64.
- Wroe A J, Cornelius I M and Rosenfeld A B. The role of nonelastic reactions in absorbed dose distributions from therapeutic proton beams in different medium Med. Phys. (2005= 32 37–41.
- Newhauser W D and Durante M 2011 Assessing the risk of second malignancies after modern radiotherapy Nat. Rev. Cancer 11 438–48.
- Wayne D Newhauser and Rui Zhang. The physics of proton therapy. Phys. Med. Biol. 60 (2015) R155.
- Aswin Hoffmann, Bradley Oborn, Maryam Moteabbed, Susu Yan et al, MR-guided proton therapy: a review and a preview. Radiation Oncology (2020) 15:129.
- E. Collings et al. Accelerators, Gantries, and Magnets for PBT. Front. Oncol., (2022). https://doi.org/10.3389/fonc.2021.737837.
